When Your Child Needs a Chest Tube
The pleural space is the area between the lung and the chest wall. If air, blood, or fluid gets into this space, it can be a problem. This air, fluid, or blood can cause one or both lungs to collapse, which makes breathing difficult. A chest tube can drain the pleural space. This tube is soft and flexible. Your child may need a chest tube to prevent their lung from collapsing. Or they may need it to allow the lung to expand after collapsing.
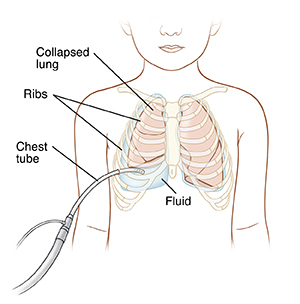 |
| A chest tube drains fluid from the pleural space. |
What are reasons for a chest tube?
Your child may need a chest tube:
-
After lung or heart surgery
-
Due to fluid or air in the pleural space from a lung infection (pneumonia)
-
Because of a problem with the lungs at birth
-
Due to a collapsed lung
-
Due to fluid or air in the pleural space from an injury or trauma.
Helping your child prepare for the procedure
You can help your child have a better experience by preparing them in advance. How you do this depends on your child’s needs. (Of course, this may not be possible if the procedure needs to be done in an emergency.)
-
Explain the procedure to your child in brief and simple terms. Younger children tend to have shorter attention spans, so do this shortly before the procedure. Older children should be given more time to understand the procedure in advance.
-
If your child will be awake during the procedure, describe how it will feel as best you can. Also, prepare your child for what to expect afterward. Let your child to ask questions.
-
Use play when helpful. This can involve role-playing with a child’s favorite toy or object. Older children may want to see pictures or a video that show them clearly what will happen during the procedure.
The procedure to place the tube
A healthcare provider places a chest tube in the operating room after surgery while your child is still asleep or sedated. This can also happen in an emergency or radiology department, or at the hospital bedside typically in the intensive care unit (ICU). The procedure takes less than 30 minutes. Here’s what you can expect:
-
Your child will first get pain medicine. Local anesthesia numbs the skin where the chest tube is placed. Your child may also get medicine to make them sleepy and relaxed. This is delivered by a mask or an IV (intravenous) line.
-
A small incision is made under a rib into the area between your child’s lung and its lining, where the tube will be placed.
-
The healthcare provider may use ultrasound, which shows pictures of the inside of your child’s body. These pictures help the healthcare provider place the tube.
-
The long, flexible tube is hooked up to a suction device.
-
The healthcare provider may stitch the tube to the skin. The site is then covered with a bandage (dressing).
-
The healthcare provider may do an X-ray to help confirm that the tube is in the right position.
After the placement procedure
-
Your child is given pain medicine by mouth or by IV line. An older child may have a patient-controlled analgesia (PCA) pump attached to the IV line. This allows your child to give themself pain medicine.
-
The drainage tube is connected to a container on the floor. This container holds sterile water. It makes a bubbling sound during suctioning.
-
Your child may need antibiotics to prevent or treat infection.
-
Your child usually has the tube in place for 1 to 4 days, depending on why it was needed. Once the fluid, blood, or air is gone, the tube is removed. This is often done at the bedside.
-
Your child may get pain medicine before the tube is removed.
-
Depending on your child’s condition, you may be able to take them home after the tube is removed.
-
Follow up with the healthcare provider within 48 hours, or as instructed by your provider. At this time, the healthcare provider will check that the incision is healing and may take more X-rays to check for fluid and how well the lung is recovering.
Helping your child after the procedure
After the procedure, you can help with drainage or healing by:
-
Encouraging deep breathing and coughing
-
Encouraging your child to move and walk around
-
Asking the healthcare provider about safe activities for your child
-
Feeding your child normal foods, if the healthcare provider says it’s OK
Caring for the incision
After the healthcare provider removes the tube, stitches may be used to close the incision. Or the incision is allowed to close by itself. Then a dressing is placed over the incision and kept in place for 48 hours, followed by use of an adhesive bandage. Here are some guidelines for wound care:
-
Once a scab has formed, you can leave the area open to the air to help with healing.
-
Your child may shower, but not bathe until a full scab has formed.
-
After the incision has healed, your child may have a small permanent scar.
Risks and possible complications
While your child is in the hospital, healthcare providers will watch for any problems that arise from having a chest tube. These are rare but can include:
-
Air leak
-
Infection
-
Reactions to anesthesia or medicines
-
Bleeding
-
Fluid in the lungs as lung expands
-
Tube can be placed in the wrong place and need to be repositioned
-
Damage to the lung
Call 911
Call 911, if your child has any of the following:
-
Grunting while breathing
-
Sudden chest pain, or shoulder or neck pain
-
Fast breath or nostrils opening wide to get air
-
Skin on neck or between ribs pulling in with each breath
-
Unusual restlessness, crying, or irritability
-
Fainting
-
Shortness of breath
Online Medical Reviewer:
Ronald Karlin MD
Online Medical Reviewer:
Scott Aydin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Date Last Reviewed:
9/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.