Scar Revision: Z-Plasty
A scar is a mark left after a wound has healed. In some cases, scar revision surgery can help improve the look of a scar or make it less visible. If the scar tissue is tight and restricts movement of the skin, revision can release or improve this. Z-plasty is a method for scar revision. While this procedure is a commonly used plastic surgical method, it may not be a good choice for people with certain medical conditions or behaviors that affect blood flow to the skin. These include poorly controlled diabetes, previous skin irradiation, peripheral vascular disease, and smoking. Your healthcare provider will discuss risk factors with you before a surgical decision is made.
Preparing for surgery
Prepare for the surgery as you have been told. Also:
-
Tell your healthcare provider about all prescription and over-the-counter medicine you take. This also includes herbs and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, and daily aspirin. You may need to stop taking some or all of them before surgery.
-
If you smoke, stop smoking or vaping before surgery. Tobacco and nicotine can slow wound healing. Don't smoke or vape after the surgery. Ask your healthcare provider for help to quit.
-
Follow any directions you are given for not eating or drinking before surgery. (If you have been told to take medicine, take them with a small sip of water.)
The day of surgery
Before the procedure, you will be asked to sign an informed consent form for both surgery and anesthesia. These forms will give information on the procedure. It will also list the risks, benefits, and alternatives to the procedure. You can ask questions before you sign the forms. Make sure all of your questions are answered before you sign the forms.
The surgery takes 1 to 3 hours. You may go home the same day. Or you may stay 1 or more nights.
Before the surgery begins
-
An IV (intravenous) line will be put into a vein in your arm or hand. This line delivers fluids and medicines.
-
You will be given medicine (anesthesia) to keep you free of pain during the surgery. You may receive sedation. This medicine makes you relaxed and sleepy. Local anesthesia will be injected to numb the body parts to be worked on. In certain cases, general anesthesia is used instead. This puts you into a state like deep sleep during the surgery. With general anesthesia, a tube may be inserted into your throat to help you breathe. The anesthesiologist will discuss your choices with you.
During the surgery
-
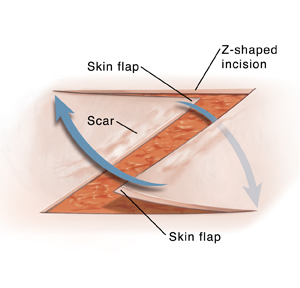
A Z-shaped incision (cut) is made through the scar tissue and some healthy skin. If the scar was very large, more than 1 Z-shaped incision may be made.
-
The Z-shape creates pointed flaps of skin. The pointed flaps of skin are arranged to break up the scar and lessen skin tightness. Once the flaps are in place, the incisions are closed with stitches. Some stitches may be placed under the skin and are absorbed later by your body.
-
The surgical site is covered with a bandage.
After the surgery
You will be taken to the PACU (postanesthesia care unit) to be watched as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. You will be given medicine to manage any pain or nausea. If the revision is to a large area, you may stay 1 or more nights in the hospital. Once you are ready to go home, you will be released to an adult family member or friend.
Recovering at home
Once at home, follow the instructions you have been given. Your healthcare provider will tell you when you can return to your normal routine. During your recovery:
-
Take prescribed medicines exactly as directed.
-
If advised by your healthcare provider, use a cold pack wrapped in a thin towel to relieve discomfort and control swelling. It’s important not to leave the cold pack on for too long or use an unwrapped ice pack because both of these actions can damage your skin. Put the pack over your bandages for no more than 10 minutes at a time. Then, leave it off for at least 20 minutes. Repeat this as often as needed during waking hours until swelling starts to improve.
-
Follow all instructions from your healthcare provider for taking care of the incision. Leave the bandage in place until you are told to remove or change it. Once you can change your bandage, do so every 24 hours or as directed. Also replace the bandage whenever it gets wet or dirty. Wash your hands before and after changing the bandage.
-
Follow your healthcare provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause incisions to be covered with water until your healthcare provider says it’s OK. Don’t apply lotions, creams, or ointments to the area until after it's fully healed.
-
Don't get dirt or sweat on your incisions. If stitches get damp, pat them dry. Change your bandage if it gets wet or soiled.
-
Keep the skin moist and lubricated after it heals. Apply mineral oil or lotion daily for 3 to 4 months, or as your healthcare provider advises.
-
Don't pick at scabs. They help protect the wound.
-
Keep the surgical area out of the sun. Cover it when you go outside. When your healthcare provider says you can, use sunscreen with a high level of protection on the area. Sunburn or sun exposure can increase scarring.
-
Don't do any exercise or movement that stretches the repaired skin until your healthcare provider says it’s OK. Talk with your healthcare provider about what movements are safe to do and which you should not do during your recovery.
When to call the healthcare provider
Call the healthcare provider right away if any of the following occur:
-
A fever of 100.4° F ( 38°C ) or higher, or as directed by your healthcare provider
-
Increased soreness, pain, or tenderness after 24 hours
-
A red streak, increased redness, or puffiness of the surgical site
-
White, yellowish, or bad-smelling discharge from an incision
-
Bleeding that doesn't stop even when you put pressure on the site for a few minutes
-
Opening of the edges of an incision
Follow-up care
You will have follow-up visits so your healthcare provider can see how well you’re healing. If you have stitches that need to be removed, this will be done at 1 of these visits. Your healthcare provider will also check on the results of your surgery. Let your healthcare provider know if you have any questions or concerns.
Risks and possible complications
Risks and possible complications include: